









DUE THE THE OUTBREAK OF THE CORONAVIRUS (COVID-19) THIS EVENT HAS BEEN POSTPONED UNTIL FURTHER NOTICE.
AOC cordially invites you to join us for a custom knee implant Q&A presentation with Joint Replacement Specialist Dr. Matthew Barber
WHEN: Thursday, April 2nd, 2020 at 5:30 PM
WHERE: Daphne Health Actions, 2102 US Highway 98, Ste K, Daphne AL, 36526
Please RSVP to Shauna Dean by March 29th, 2020:
EMAIL: shauna_dean@alortho.com
PHONE: 251-410-3686


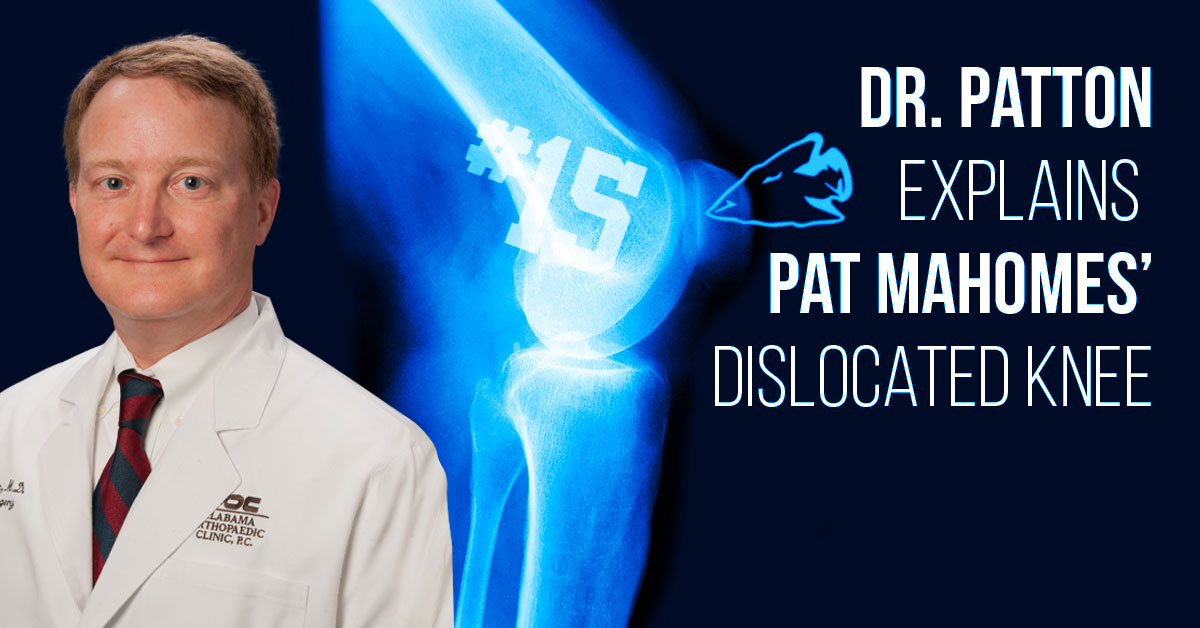
During a quarterback sneak against Denver, Patrick Mahomes dislocated his right patella (knee cap). The combination of a twist to the knee and the collision caused the patella to dislocate laterally.
It was gently put back in place by the medical staff on the field by extending the knee and pushing the patella back in place. This immediately reduced his pain. X-rays and MRI were needed to evaluate for any fracture of bone and to assess the ligaments that help keep the knee cap from dislocating again.
These studies also evaluated the alignment of the leg to see if he has predisposing factors for dislocation. Initial reports have stated that there is minimal damage to the structures around the patella. This could mean less missed playing time following rehabilitation.




Mr Brees’ thumb injury is a fairly common one amongst athletes at all levels. Commonly referred to as gamekeeper’s or skier’s thumb, it involves a rupture of one of the key stabilizing ligaments to the thumb MCP joint (knuckle). This ligament is critical for activities that involve strong pinch or grip or grasp. This used to be a season-ending injury, however recent advancements in surgical techniques have greatly reduced recovery times. More recently multiple high-level professional athletes, including Mike Trout in 2017, have been able to return to play within the 6-8 week range.
Dr. Barber visited the Uncle Henry morning show on Friday (August 16th) to discuss joint replacement advances including robotic surgery, custom implants and outpatient options.

















The treatment of meniscal tears has advanced over the years. Forty years ago it would not have been unheard of to excise in an open fashion the entire meniscus. This led to the development of arthritis earlier than was expected. With the development of knee arthroscopy and the small instruments to work inside the knee, debrided (shaving) just the tear became more common. This allowed meniscal tissue to be preserved.
As studies have shown the benefits of preserving meniscal tissue, repairing the meniscus, if possible, has become a goal. Several techniques including “outside-in”, “inside-out”, and “all inside” were developed. The term “all-inside” means the stiches are tied or the device deploys inside the knee without the need for additional incisions. This is also known as “all arthroscopic.” Regardless of the technique, the goal is to repair the meniscus in a stable manner so that early range of motion and healing are possible.
The indications for repair continue to expand with tears greater than one centimeter in the area of good blood supply and in patients less than 40 being common. Additionally, repairs at the time of ACL reconstruction, vertical tears, and acute tears also being good candidates for repair. As the technology improves the candidates for repair are expanding.
When meniscal tissue is severely lost in young patients with good alignment, intact ligaments, and no significant arthritis, meniscal transplant has been developed as an option. Taking a meniscus from a young donor and either suturing it in the knee with or without a piece of bone attached can restore needed meniscus tissue. Long term studies of meniscal transplant are on-going. Hopefully as studies are produced and technology develops, preservation of meniscal tissue will continue to advance in the hope of preserving the articular cartilage and normal biomechanics of the knee.





Knee arthroscopy (the placing of a small camera into the knee and performing surgery through small holes) is one of the most common orthopaedic procedures performed in the United States. Over 900,000 of these are performed each year, and over half are done to operate on a torn meniscus.1 The meniscus is a C-shaped cartilage structure on the inside (medial) and outside (lateral) of the knee. Acute traumatic tears of the meniscus are often caused by sporting activities or an activity where there is a sudden twisting of the knee. Hyperflexion of the knee can cause meniscal tears also. Degenerative type tears can be caused by age or untreated instability of the knee.
The meniscus serves an important function in the knee by acting as a cushion to the underlying joint cartilage called the articular cartilage. Loss of meniscus tissue through tearing or surgical removal can lead to increases in stress placed upon the articular cartilage. This can lead to arthritis. Additionally, the meniscus acts as a joint stabilizer. Loss of the meniscus can place increased stress on the major ligaments of the knee such as the anterior cruciate ligament (ACL). Therefore, preserving as much meniscus as possible is a goal for orthopaedic surgeons.
The diagnosis of a meniscal tear requires taking a history, performing a physical exam of the entire knee and surrounding structures, and performing additional diagnostic tests. As stated above, a history of a twisting injury or hyperflexion injury of the knee can lead to a meniscal tear. Common physical exam findings include swelling of the knee, joint line tenderness on the side of the tear, and pain with certain maneuvers that the physician performs such as a McMurray’s test. (The McMurray’s test is performed by taking the knee from a flexed position to an extended position while the tibia is kept internally rotated (for the lateral meniscus) or externally rotated (for medial meniscus). McMurray described a palpable click as being “positive”.2
Diagnostic tests for evaluating a torn meniscus include X-rays of the knee, MRI and knee arthroscopy. The plain X-rays do not detect the torn meniscus, but they rule out other causes of knee pain such as loose bodies and arthritis. The most common non-surgical diagnostic test for meniscal tears is the MRI. It has a high sensitivity and does not involve radiation. MRI can detect both meniscal and ligamentous tears. The “gold standard” test for diagnosing meniscal tears is actually seeing it with knee arthroscopy. This common outpatient procedure can be performed under general or spinal anesthesia.
1Kim et al: Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011 Jun 1;93(11):994-1000.
2 McMurray TP: The semilunar cartilages. Br J Surg 1942;29(116):407–414




Have you been diagnosed with a slipped disc in your back and your doctor recommended surgery? Spinal fusion is a procedure to stabilize the spine when arthritis has led to instability of the spinal segment (2 bones around the disc). This procedure is usually done along with a laminectomy to relieve the pressure on the spinal nerves. Patients with mechanical low back pain and pain in the legs when standing or walking, may benefit from this procedure. Screws and rods are placed around the spine for stability along with bone graft for the fusion.